Delta waves are the slowest and highest amplitude waves of the sleep cycle. Delta waves can be seen in deep, dreamless sleep and during anesthesia.
Delta waves are small, very low frequency (0.5 to 4 Hz), large amplitude waves that occur predominantly in the frontal areas of the brain. Delta waves are generated by the thalamus and other parts of the brainstem. They are usually associated with deep sleep or unconsciousness but may also be observed in any stage of sleep when a person is relaxed. Delta sleep is usually associated with prominent slow-wave activity (SWA) in the EEG and high amplitude delta activity on an electroencephalogram (EEG).
Delta waves have been found to be associated with:
Deep Sleep
Unconsciousness
Anesthesia
Delta waves are the slowest brainwaves and ecg occur in deep sleep. They are so slow that they are undetectable by an electroencephalogram (EEG) unless amplified. Delta waves have a frequency of 0 to 3 cycles per second (0 – 3 Hz).
Delta waves are associated with deep, dreamless sleep. They are also associated with unconsciousness, as seen in patients under anesthesia and in coma patients.
Delta waves are usually seen as a sign of illness or injury, although they can also be present during exercise, hypnosis or meditation.
In humans, delta waves occur during slow-wave sleep (SWS), when the brain is relatively inactive.[1] SWS is a deeper stage of non-rapid eye movement sleep (NREM). It is seen on an electroencephalogram as a flattening of the form of the EEG waves called “sleep spindles” and “K complexes”, which indicates that neurons in certain regions of the brain have slowed down their electrical activity.[2] This occurs most often in cycles lasting about 90 minutes each; these cycles repeat throughout the night.[3]
Delta waves are the slowest brain waves, with ecg frequencies of under 4 hertz. They are seen in deep sleep and during coma, as well as in some brain diseases (particularly Alzheimer’s disease).
Delta waves are thought to help the brain process information that it has learned prior to sleep (e.g., storing memories), and they may also play a role in memory formation while awake. Delta waves have been shown to increase in the human brain during learning tasks involving visual or auditory stimuli.
Delta waves are very slow brainwaves that mostly occur during deep sleep. They are the longest and slowest brainwaves that you can have, and they show up when you are asleep. Delta waves are associated with deep sleep and healing, but they can also be seen when someone is in a coma or has been sedated.
Delta waves are different from other ecg brainwave frequencies because they don’t have any frequency, or amplitude. They just oscillate slowly between -4 and +4 Hz (hertz), which is equivalent to 0 and 2 hz (cycles per second). The reason why they’re called delta waves is because their frequency falls within the range of 1-4 Hz, which is below the first two letters of “delta” (D).
What does a delta wave mean on ECG?
A delta wave is a type of aberrant conduction that can be seen on an electrocardiogram (ECG). It is characterized by a sharp negative deflection on the QRS complex. Delta waves may be caused by electrolyte abnormalities or by overdose of medication such as digoxin.
Delta waves are abnormal and should not be seen in healthy individuals. They are usually seen in patients with digoxin toxicity or hypokalemia, two conditions that affect the electrical impulse conduction through the heart. A delta wave can also be seen in patients with hypothyroidism because their metabolic rate slows down and therefore the heart rate does too.
A delta wave (also known as a “delta activity”) is a slow and high-voltage wave that occurs in the electrocardiogram. It is often associated with hypothermia, cardiac arrest, or other life-threatening conditions.
A delta wave is usually a normal finding in the resting ECG in healthy individuals, but it can be present in patients with hypothermia or cardiac arrest. In some cases, the presence of this wave may indicate a myocardial infarction. However, more often than not, it is not associated with any disease process and can be considered a normal variant variant pattern.
A delta wave is a high frequency electrical ecg signal that occurs in normal heart rhythms. It is usually found in the right atrium and ventricle, but it may also be seen in other areas of the heart. A delta wave is not always visible on an electrocardiogram (ECG). It may only be seen when the heart rate is very slow or when there is another abnormality with the rhythm.
The most common cause of a delta wave is an ectopic pacemaker, which is a separate electrical impulse that causes the heart to beat independently from the sinus node. This can lead to abnormal heart rhythms and palpitations.
What disorder produces a delta wave?
The delta wave is the slowest and highest frequency brainwave. It is produced in deep sleep and characterized by slow, large amplitude waves.
The delta wave is associated with deep ecg sleep and great relaxation. A person who is dreaming also has a high amplitude delta wave activity. This is one of the reasons why you cannot remember your dreams immediately after waking up from deep sleep. There are other types of sleep disorders that can produce this type of wave such as narcolepsy and possibly night terrors.
Delta waves are the slowest, highest amplitude brain waves seen in the EEG. These waves are produced during deep sleep and also when a person is under general anesthesia.
Delta waves can be seen in normal individuals, but they are prominent in people who have certain types of epilepsy or brain damage. This type of wave is also seen in people who have had strokes or head injuries that affect certain parts of the brain. The delta wave is also known as a slow-wave potential because it occurs at an extremely slow rate (about one per second).
The delta wave is a type of brain wave ecg that occurs during deep sleep. Delta waves are the slowest and highest frequency waves occurring in the brain, measuring between 0.5 and 4 hertz (Hz). This range of frequencies is associated with deep sleep and unconsciousness.
Delta waves are most prominent in infants, children and adults under the age of 20 years old. They begin to disappear after adulthood, but can appear temporarily during times of extreme stress or fatigue.
The absence of delta waves is associated with insomnia, narcolepsy and epilepsy.
Delta Waves in Infants
In infants, delta waves are present throughout ecg sleep periods due to their immature brains not producing other types of brain waves yet. This can be problematic for infants who have difficulty sleeping because they will not produce other types of brain waves during their sleep cycles.
Delta Waves in Children
In children between the ages of two and six years old, delta waves occur at a high rate during their non-rapid eye movement (NREM) stage 3 sleep period (stage 3). This stage is known as slow-wave sleep because it consists of longer periods without rapid eye movements compared to stage 2 sleep (stages 2 and 3 together make up NREM).
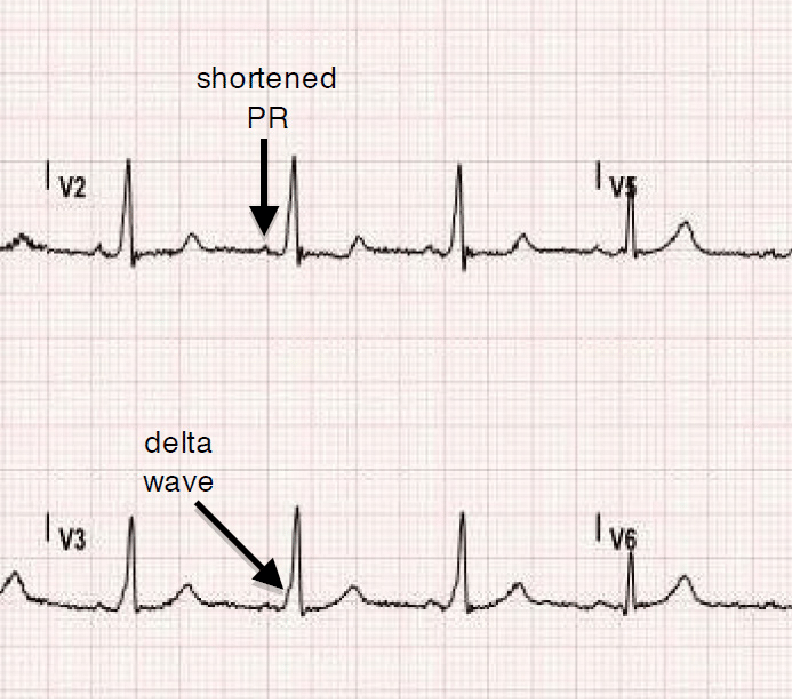
What does Wolff-Parkinson-White syndrome look like on ECG?

Wolff-Parkinson-White syndrome is a congenital disorder that affects the heart’s conduction system. It can cause an abnormal rhythm known as supraventricular tachycardia (SVT).
What does Wolff-Parkinson-White syndrome look like on ECG?
The ECG trace may show:
A rapid heart rate of 150 to 250 beats per minute
A short PR interval (0.12 second or less)
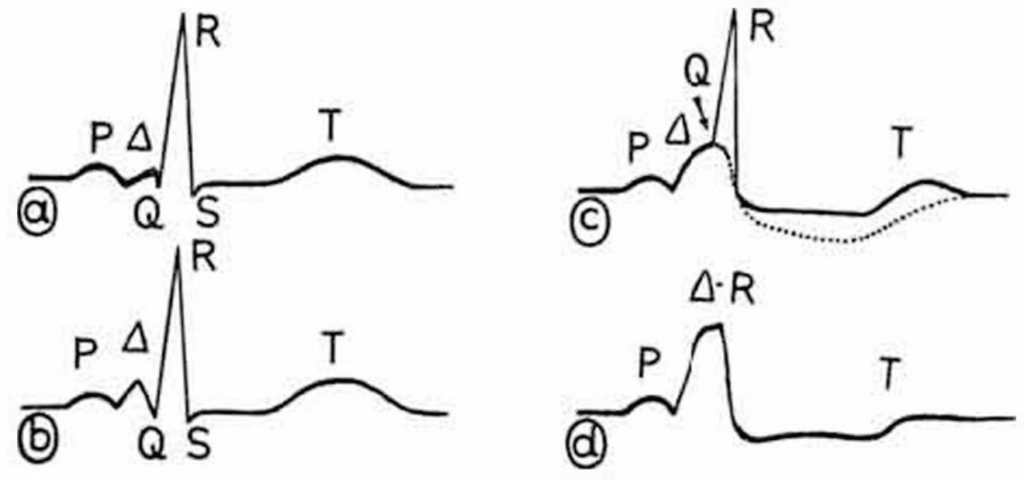
A delta wave, which is a small upward deflection in the baseline just before the QRS complex (the main electrical signal generated by your heart muscle)
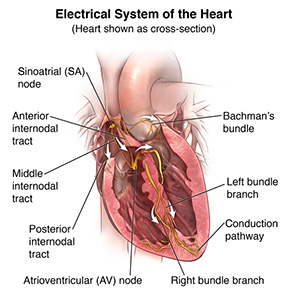
Wolff-Parkinson-White syndrome (WPW syndrome) is a condition in which an extra electrical pathway exists between the upper chambers of the heart (atria) and the lower chambers (ventricles).
The extra pathway can allow an abnormal amount of electrical current to travel through the heart. This can cause fast, irregular heartbeats (arrhythmias).
The disorder usually affects the upper chambers of the heart — the atria. It can also affect the ventricles (lower chambers of the heart).
ECG What does Wolff-Parkinson-White syndrome look like on ECG?
The pattern on ECG is:
1. PR interval less than 0.12 seconds at rest or during exercise.
2. QRS complex duration less than 0.10 seconds at rest or during exercise; however, it can be up to 0.16 seconds if there is no bundle branch block present with WPW syndrome alone.[23]
Wolff-Parkinson-White syndrome is a condition that causes an abnormal electrical pathway from the upper chambers of the heart (atria) to the lower chambers (ventricles). This electrical pathway is called an accessory pathway. Normally, the upper atria contract first and then send their electrical impulse to the lower ventricles. With Wolff-Parkinson-White syndrome, there’s an extra electrical pathway between the upper and lower chambers. This allows some of the electrical signal from the upper atria to reach the ventricles early — before it gets through the normal pathways.
A person with Wolff-Parkinson-White syndrome may have signs and symptoms such as:
Fast heartbeat (tachycardia) — usually between 140 and 200 beats per minute
Heart palpitations — awareness of a fast or irregular heartbeat
Fainting spells
What causes delta wave WPW?
ECG Delta wave WPW is a relatively rare type of congenital heart disease in which the electrical signals that control the heartbeat are abnormal. It is also known as Wolff-Parkinson-White syndrome (WPW).
In most cases, delta wave WPW causes ecg no symptoms and can be easily detected with an electrocardiogram (ECG). However, in some cases, it can lead to serious complications, including sudden cardiac arrest and other potentially life-threatening conditions.
Delta wave WPW is a rare form of Short QT Syndrome, which is a group of heart rhythm disturbances. The most common form of Short QT Syndrome causes the heart to beat too quickly and may lead to sudden death (heart attack).
Delta wave WPW occurs when the electrical signals in your heart are not synchronized correctly. This can cause the ventricles (lower chambers) of your heart to contract very early during the heartbeat cycle (ventricular pre-excitation). This will cause you to have an abnormal pattern on an EKG called delta waves.
In some cases, this can make you feel like you are having a heart attack or other symptoms like dizziness, chest pain and fainting.
ECG There are two types of delta wave WPW: type 1 and type 2. Type 1 occurs when there is an extra pathway for electrical signals from the atria (upper chambers) to travel through before reaching the ventricles, while type 2 occurs when there is no extra pathway present but instead there are changes within the muscle cells themselves that allow them to contract earlier than normal during each heartbeat cycle.
The cause of Delta wave pre-excitation is a mutation in the genes that control your heart’s electrical system. It can be passed down through families.
In some cases, there’s no family history of the condition. Scientists ecg aren’t sure what causes these cases, but they think they might be due to random mutations in the genes that control your heart’s electrical system.
The most common type of Delta wave pre-excitation is caused by a mutation in a gene called KCNQ1, which controls the flow of potassium into and out of your heart cells (called cardiomyocytes). When this gene mutates, it causes a short circuit in the electrical system that regulates your heart rate and rhythm — like when you plug two wires together with no protective covering on them. This short circuit causes abnormal electrical activity that leads to irregular heartbeats or arrhythmias.
Is WPW life threatening?

WPW is not life threatening, but it can be dangerous if left untreated. It is important to know the symptoms of WPW and how to treat it.
Symptoms of WPW
The most common symptom of WPW is ventricular tachycardia (VT), which is a very fast heartbeat that can last for several minutes. Another symptom that is less common but more serious is ventricular fibrillation (VF), which can lead to death if not treated quickly.
Other symptoms include:
Sudden loss of consciousness or feeling dizzy or lightheaded
Chest pain or pressure in the chest
ECG Shortness of breath or difficulty breathing
WPW is an inherited condition. It is present at birth, but it only becomes life-threatening if the individual has a heart attack or develops other complications. In some cases, the patient may experience symptoms during their lifetime.
In the majority of cases, WPW is not life threatening and does not require treatment. However, it can be if there is an underlying heart condition or if you have had a previous heart attack.
WPW happens when there is a problem with your ecg heart’s electrical system. Your heart has an electrical system that controls its beating pattern and sends messages to your body that allow it to function properly.
The normal sequence of events in this process is as follows:
Your heart muscles contract at regular intervals and pump blood out of your heart into your arteries (the blood vessels in your body). This pumping action moves blood through the body and allows oxygen to reach all parts of your body so they can function normally. When you breathe out, carbon dioxide leaves the body through your lungs and returns to your heart through veins on its way back to the lungs for re-oxygenation. The oxygenated blood then flows back into your heart through veins from all over your body.
The answer is that WPW is not life threatening in the sense that you will die from it. However, it can cause sudden cardiac arrest and death if not treated.
People with WPW have an increased risk of having a life-threatening rhythm disturbance called torsades de pointes. This is a type of abnormal heart rhythm (arrhythmia) that can lead to sudden death if it goes untreated.
The most common cause of sudden deaths in people with WPW is torsades de pointes, which occurs when there is an abnormality in the electrical pathways within the heart.
Can WPW cause sudden death?
The short answer is yes. WPW is a form of heart rhythm problem that can cause sudden cardiac death, but it’s not the only one and it’s not even the most common.
Sudden cardiac death is most often caused by a fatal heart rhythm called ventricular fibrillation (VF). VF causes an irregular and chaotic heartbeat that prevents blood from flowing through the heart and out to other parts of the body. This can lead to sudden collapse, loss of consciousness and death.
If you have WPW, your doctor may ecg prescribe medication to slow down your heart rate or treat other symptoms like palpitations or dizziness. But with careful monitoring, you can live a full life without worry about sudden death — as long as you stay aware of your condition and take good care of yourself.
Sudden cardiac death is a rare occurrence in patients with WPW syndrome. In fact, sudden death is more likely to occur in people who do not have WPW than those who do. However, although uncommon, sudden death can occur in some patients with WPW syndrome if they experience ventricular tachycardia (VT) or ventricular fibrillation (VF).
Some patients with WPW may experience asymptomatic episodes of VT or VF that resolve spontaneously without intervention. These episodes may occur once or multiple times over a period of weeks or years. This type of event is known as paroxysmal supraventricular tachycardia (PSVT) and it may be associated with palpitations and lightheadedness but rarely causes any significant symptoms.
However, some people with WPW ecg may experience symptoms such as dizziness and shortness of breath during these episodes. This type of event is known as polymorphic ventricular tachycardia (PMVT). If these symptoms are present in someone who has a history of having had PSVT before, it’s important to seek medical attention immediately because they could indicate a serious problem that requires immediate treatment.
WPW syndrome can cause sudden cardiac death. However, the risk of sudden death is not as high as with other types of arrhythmias.
The most common symptoms of WPW syndrome are chest pain and dizziness. These symptoms tend to occur when you’re standing up or exercising. You may also experience palpitations (the feeling that your heart is beating too fast or too hard) or fainting when you stand up quickly.
It’s important to note that these symptoms aren’t specific for WPW syndrome and could also be caused by other conditions, such as coronary artery disease and abnormal heart valve function.
Who is at risk for WPW?
WPW is most commonly due to a genetic ecg condition called long QT syndrome (LQTS). WPW occurs in about 1 in 2,000 people. It affects men and women equally and can be inherited from either parent.
A family history of sudden cardiac death is the strongest risk factor for WPW. At least one other person in your family with the disorder increases your risk of having WPW by 30%. If you have WPW, you have an increased risk of sudden cardiac death compared to the general population.
WPW is more common in young people, particularly in men. It can also occur more often in people with certain heart conditions, such as Wolff-Parkinson-White syndrome, atrial fibrillation and other irregular heartbeats.
Women are more likely to have WPW than men. Women ecg tend to have the condition at a younger age than men do.
If you have WPW and an episode of SVT or AF, you’re at risk for a fast heartbeat that may lead to sudden cardiac arrest (SCA). People with WPW are also at higher risk of having other types of abnormal heart rhythms that may cause SCA.
If you experience symptoms of SVT or AF, seek medical attention immediately.
Is WPW an emergency?
WPW is a type of tachycardia. Tachycardias are a group of heart rhythms that are fast enough to interfere with blood flow through the heart.
If you’re having a sudden or ongoing episode of WPW, it’s an emergency situation. Call 911 or ecg go to an emergency room immediately.
Some episodes of WPW may be so mild that they don’t require treatment and resolve on their own. But because WPW can cause serious complications, it’s important that you know how to recognize the signs and symptoms and act quickly if needed.