Geriatric syndrome is a term used to describe a collection of health conditions commonly found in older adults. These conditions often occur concurrently and can have a significant impact on an individual’s overall well-being. In this blog post, we will explore the key aspects of geriatric syndrome and discuss effective management strategies.
- Definition and Common Conditions: Geriatric syndrome encompasses a range of conditions that are prevalent in older adults, including:
a) Falls and balance problems
b) Cognitive impairment and dementia
c) Urinary incontinence
d) Functional decline and disability
e) Polypharmacy and adverse drug reactions
f) Malnutrition and weight loss
g) Depression and social isolation
- Risk Factors: Several factors contribute to the development of geriatric syndrome, including:
a) Age-related physiological changes
b) Chronic medical conditions
c) Medications and their interactions
d) Environmental hazards
e) Cognitive decline
f) Social and economic factors
- Impact on Older Adults: Geriatric syndrome can significantly affect the quality of life for older adults. Some of the common consequences include:
a) Increased risk of falls and fractures
b) Decline in cognitive abilities and independence
c) Reduced mobility and functional limitations
d) Higher rates of hospitalization and institutionalization
e) Impaired social interactions and mental health issues
- Management Strategies: To effectively address geriatric syndrome, a comprehensive and multidisciplinary approach is essential. Here are some key management strategies:
a) Comprehensive geriatric assessment: An in-depth evaluation of medical, functional, cognitive, and social aspects to identify underlying issues.
b) Medication review: Regular assessment of medications to minimize polypharmacy and potential adverse effects.
c) Physical activity and balance training: Exercise programs to improve strength, balance, and mobility.
d) Nutrition optimization: Ensuring a well-balanced diet to prevent malnutrition and weight loss.
e) Cognitive stimulation: Activities that promote mental engagement and help maintain cognitive function.
f) Social support and engagement: Encouraging social interactions and addressing isolation and depression.
g) Home modifications: Identifying and addressing environmental hazards to reduce the risk of falls and injuries.
h) Care coordination: Collaboration among healthcare professionals to ensure holistic and coordinated care.
Geriatric syndrome encompasses a range of common health conditions affecting older adults. Understanding the key aspects of geriatric syndrome and implementing appropriate management strategies is crucial for promoting healthy aging and enhancing the well-being of older individuals. By addressing these conditions comprehensively, we can improve the quality of life and functional independence of older adults, allowing them to age gracefully and enjoy a higher level of well-being.
What are some common geriatric syndromes?
Geriatric syndromes are a set of common health conditions that frequently affect older adults. These syndromes are not specific diseases but rather a collection of symptoms and functional impairments that often occur together. In this blog post, we will discuss some of the most prevalent geriatric syndromes and their key characteristics.
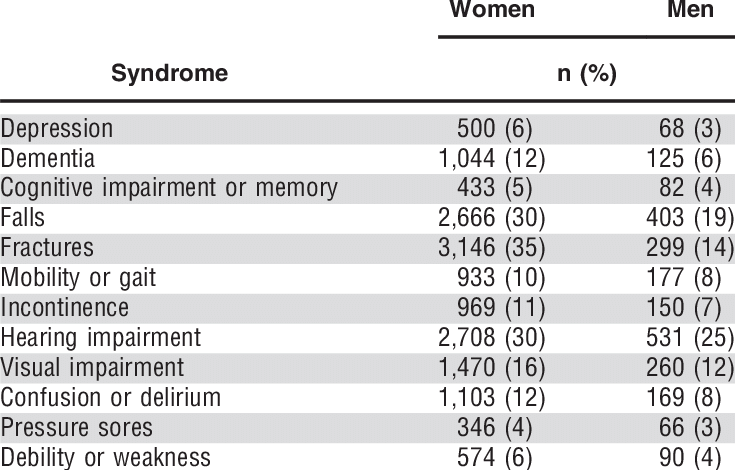
- Falls: Falls are a significant concern among the elderly population. Age-related changes in balance, muscle strength, and coordination can increase the risk of falls, leading to injuries such as fractures or head trauma. Identifying fall risk factors and implementing preventive measures are crucial for maintaining the safety and well-being of older adults.
- Cognitive Impairment: Conditions like dementia and Alzheimer’s disease are characterized by a decline in cognitive abilities, including memory, thinking, and problem-solving skills. Cognitive impairment can impact daily functioning, decision-making, and independence. Early detection, appropriate management, and support systems are essential for individuals affected by cognitive decline.
- Urinary Incontinence: Many older adults experience urinary incontinence, which refers to the involuntary loss of urine. This condition can be caused by a variety of factors, such as weakened pelvic floor muscles, bladder dysfunction, or certain medications. Effective management strategies include lifestyle modifications, pelvic floor exercises, and medical interventions.
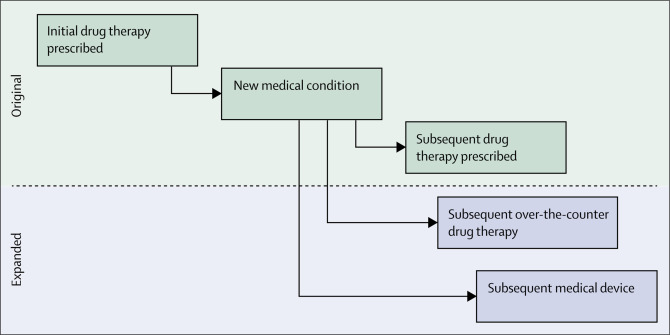
- Polypharmacy: Polypharmacy is the use of multiple medications by an individual. Older adults are particularly susceptible to polypharmacy due to the presence of multiple chronic conditions requiring different treatments. This can increase the risk of adverse drug reactions, drug interactions, and medication non-adherence. Regular medication reviews and communication with healthcare providers are essential to optimize drug therapy.
- Pressure Ulcers: Also known as bedsores, pressure ulcers are skin injuries that occur due to prolonged pressure on bony areas of the body. Immobility, frailty, and poor nutrition can contribute to the development of pressure ulcers. Preventive measures, such as regular repositioning, adequate nutrition, and maintaining skin hygiene, are vital for minimizing the occurrence of pressure ulcers.
- Geriatric Depression: Depression is common among older adults and often goes undiagnosed. Factors like social isolation, loss of loved ones, and chronic health conditions can contribute to the development of geriatric depression. Early identification, psychotherapy, and pharmacological interventions can significantly improve the mental well-being of older adults.
- Sensory Impairments: Age-related hearing loss and vision problems are prevalent among older adults. These sensory impairments can impact communication, social interactions, and overall quality of life. Regular hearing and vision screenings, assistive devices, and environmental modifications can help manage these conditions effectively.
Understanding these common geriatric syndromes can assist healthcare providers, caregivers, and older adults themselves in recognizing the associated challenges and implementing appropriate interventions. By addressing these syndromes proactively, we can enhance the health, independence, and overall well-being of older individuals.
What are the 7 geriatric syndromes?

As individuals age, they may experience a variety of health conditions and challenges that are more prevalent in older adults. These conditions, known as geriatric syndromes, encompass a range of physical, cognitive, and functional issues that can significantly impact an older person’s well-being. In this article, we will explore the seven most common geriatric syndromes and provide a brief overview of each.
- Falls: Falls are a major concern among the elderly and can result in serious injuries such as fractures or head trauma. Factors contributing to falls include decreased muscle strength, balance problems, medication side effects, and environmental hazards. Preventive measures, such as regular exercise, home modifications, and medication review, can help reduce the risk of falls.
- Delirium: Delirium refers to an acute state of confusion and cognitive decline. It can be caused by underlying medical conditions, infections, medication changes, or surgery. Prompt identification and addressing the underlying cause are crucial for managing delirium in older adults.
- Urinary Incontinence: Urinary incontinence is the involuntary loss of bladder control, leading to leakage of urine. Common causes include weakened pelvic floor muscles, neurological disorders, and urinary tract infections. Treatment options range from lifestyle modifications to medication or surgical interventions, depending on the underlying cause.
- Cognitive Impairment and Dementia: Cognitive impairment encompasses a spectrum of conditions, including mild cognitive impairment (MCI) and dementia. MCI involves a decline in cognitive abilities beyond what is expected with normal aging, while dementia refers to a more severe and progressive cognitive decline that affects daily functioning. Early detection, proper diagnosis, and appropriate management strategies are essential for individuals with cognitive impairment or dementia.
- Pressure Ulcers: Pressure ulcers, also known as bedsores, are localized injuries to the skin and underlying tissue caused by prolonged pressure or friction. Older adults with limited mobility or who spend significant time in bed or chairs are particularly at risk. Preventive measures such as regular repositioning, proper nutrition, and skincare can help reduce the occurrence of pressure ulcers.
- Polypharmacy: Polypharmacy refers to the use of multiple medications by an individual, often resulting in adverse drug interactions or side effects. Older adults are more susceptible to polypharmacy due to the presence of multiple chronic conditions. Regular medication review, communication with healthcare providers, and deprescribing when appropriate can help mitigate the risks associated with polypharmacy.
- Functional Decline: Functional decline involves a gradual loss of independence in performing activities of daily living (ADLs) and instrumental activities of daily living (IADLs). ADLs include basic self-care tasks like bathing and dressing, while IADLs encompass more complex activities such as managing finances or using transportation. Rehabilitation, assistive devices, and support from caregivers can aid in maintaining or improving functional abilities.
- Geriatric syndromes are prevalent among older adults and require comprehensive assessment, management, and preventive strategies. By recognizing and addressing these syndromes, healthcare providers, caregivers, and older individuals themselves can work together to optimize health and well-being in the aging population.
Geriatric syndromes are prevalent among older adults and require comprehensive assessment, management, and preventive strategies. By recognizing and addressing these syndromes, healthcare providers, caregivers, and older individuals themselves can work together to optimize health and well-being in the aging population.
What are the symptoms of geriatric syndrome?
Geriatric syndrome refers to a collection of health conditions commonly experienced by older adults. This syndrome is not caused by a specific disease but rather a combination of factors related to aging. In this blog post, we will explore the symptoms of geriatric syndrome and discuss strategies for managing and improving the overall well-being of older individuals.
Symptoms of Geriatric Syndrome:
- Functional Decline: Older adults with geriatric syndrome may experience a decline in their ability to perform daily activities independently. This can include difficulties with mobility, balance, dressing, grooming, and feeding.
- Cognitive Impairment: Memory loss, confusion, disorientation, and difficulty concentrating are common symptoms associated with geriatric syndrome. These cognitive changes can significantly impact an individual’s quality of life.
- Falls: Older adults with geriatric syndrome are at a higher risk of experiencing falls due to factors such as muscle weakness, impaired balance, and reduced coordination. Frequent falls can lead to injuries, fractures, and a fear of falling, further limiting mobility.
- Incontinence: Geriatric syndrome often includes urinary and fecal incontinence, which can be distressing for older adults. Bladder control issues may result from weakened pelvic muscles and reduced bladder capacity, while bowel incontinence can be linked to age-related changes in the digestive system.
- Malnutrition: Poor nutrition and unintentional weight loss are prevalent symptoms of geriatric syndrome. Older adults may experience a decrease in appetite, difficulty chewing or swallowing, or inadequate access to nutritious food, leading to malnourishment and its associated health complications.
Management Strategies:
- Multidisciplinary Care: Older adults with geriatric syndrome benefit from a team-based approach involving healthcare professionals such as physicians, nurses, physical and occupational therapists, and dietitians. This collaborative effort ensures a comprehensive assessment and tailored treatment plan.
- Medication Review: Older individuals often take multiple medications, which can contribute to adverse effects and drug interactions. Regular medication reviews with a healthcare provider help identify and address any medication-related issues.
- Fall Prevention: Implementing measures to minimize the risk of falls is crucial. This includes removing tripping hazards at home, installing grab bars in bathrooms, using assistive devices like canes or walkers, and participating in exercise programs aimed at improving strength and balance.
- Cognitive Stimulation: Engaging in mentally stimulating activities, such as puzzles, reading, or socializing, can help maintain cognitive function and slow down cognitive decline.
- Nutritional Support: Older adults should be encouraged to consume a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. In some cases, dietary supplements may be recommended to address specific nutrient deficiencies.
Geriatric syndrome encompasses a range of symptoms that older adults commonly experience as they age. By recognizing these symptoms and implementing appropriate management strategies, healthcare professionals and caregivers can help enhance the well-being and overall quality of life for older individuals.
What are the 5 geriatric giants?
Aging is a natural process that brings both opportunities and challenges. Among the challenges faced by older adults, five common conditions known as the “Geriatric Giants” significantly impact their overall well-being. In this article, we will explore these giants and their effects on aging individuals.
- Falls: Falls pose a significant risk to older adults, leading to injuries, fractures, and loss of independence. Factors such as muscle weakness, impaired balance, and reduced vision increase the likelihood of falls. To prevent falls, regular exercise, home modifications, and awareness of potential hazards are crucial.
- Cognitive Decline: Age-related cognitive decline, including dementia and Alzheimer’s disease, can significantly impact an individual’s memory, thinking, and daily functioning. Engaging in mentally stimulating activities, maintaining a healthy lifestyle, and seeking medical advice for early detection are vital in managing cognitive decline.
- Incontinence: Urinary and fecal incontinence are common problems among older adults, affecting their dignity and quality of life. Lifestyle modifications, pelvic floor exercises, and medical interventions can help manage incontinence, providing relief and improving daily activities.
- Immobility: Reduced mobility, often resulting from age-related conditions or chronic illnesses, can limit older adults’ independence and physical functioning. Regular exercise, physical therapy, assistive devices, and home modifications can enhance mobility and prevent further decline.
- Polypharmacy: Polypharmacy refers to the use of multiple medications by an individual, which can lead to adverse drug interactions, side effects, and medication errors. To address this issue, healthcare providers should regularly review and simplify medication regimens, promote communication between healthcare professionals, and encourage patient education.
The Geriatric Giants—falls, cognitive decline, incontinence, immobility, and polypharmacy—represent significant challenges faced by older adults. Recognizing these giants and implementing preventive measures, lifestyle modifications, and appropriate medical interventions can help mitigate their impact, enhancing the overall well-being and quality of life for aging individuals.
What are the 5 frailty syndromes?
Frailty syndromes are a set of age-related conditions that affect older adults, leading to decreased physical and cognitive function. Here are five common frailty syndromes:
- Sarcopenia: Sarcopenia refers to the loss of muscle mass and strength associated with aging. It can result in reduced mobility, balance problems, and increased risk of falls.
- Frailty: Frailty is a state of increased vulnerability to stressors due to age-related decline in physiological reserves. It is characterized by weakness, fatigue, decreased physical activity, and impaired functioning in multiple domains.
- Cognitive Impairment: Cognitive impairment, including mild cognitive impairment (MCI) and dementia, affects memory, thinking, and decision-making abilities. It can significantly impact daily functioning and independence.
- Falls and Fall-Related Injuries: Falls are a common problem among older adults and can lead to severe injuries such as fractures and head trauma. They are often caused by a combination of factors, including muscle weakness, impaired balance, and environmental hazards.
- Polypharmacy: Polypharmacy refers to the concurrent use of multiple medications, which is common among older adults with multiple chronic conditions. It increases the risk of adverse drug reactions, drug interactions, and medication non-adherence.
These frailty syndromes highlight the importance of addressing age-related changes through proactive measures such as regular physical activity, a balanced diet, cognitive stimulation, medication review, and fall prevention strategies. By understanding and managing these syndromes, older adults can maintain their independence and quality of life as they age.
What are the 6 geriatric syndromes?
Geriatric syndromes are a set of common health conditions that affect older adults. Here are the six geriatric syndromes:
- Falls: Falls are a significant concern among older adults, as they can lead to serious injuries and a decline in overall health. Preventive measures such as regular exercise, home modifications, and medication review can help reduce the risk of falls.
- Cognitive impairment: Cognitive impairment encompasses a range of conditions, including mild cognitive impairment and dementia. Early detection, proper management, and support systems are essential for individuals with cognitive impairment and their caregivers.
- Incontinence: Incontinence refers to the loss of bladder or bowel control. It can significantly impact an individual’s quality of life. Treatment options include lifestyle modifications, medications, and exercises to strengthen the pelvic floor muscles.
- Polypharmacy: Polypharmacy occurs when individuals take multiple medications, which can lead to drug interactions and adverse effects. Regular medication reviews and communication with healthcare providers are crucial to minimize risks associated with polypharmacy.
- Malnutrition: Malnutrition is a common issue in older adults and can result from various factors such as poor appetite, difficulty swallowing, or chronic conditions. A well-balanced diet, regular monitoring, and addressing underlying health conditions are vital in preventing and managing malnutrition.
- Depression: Depression affects many older adults but often goes undiagnosed and untreated. It can have a profound impact on mental and physical health. Early recognition, social support, counseling, and, if necessary, medication can help manage depression in older adults.
These geriatric syndromes require a multidisciplinary approach involving healthcare professionals, caregivers, and the individuals themselves. By addressing these syndromes, we can improve the overall well-being and quality of life for older adults.
