What Size Hiatal Hernia Needs Surgery; A hiatal hernia is a common medical condition that occurs when a portion of the stomach protrudes through the diaphragm and into the chest cavity. While many people may have a small hiatal hernia without even realizing it, there are cases where the condition can cause discomfort, pain, and other complications. In such instances, surgery may be considered as a treatment option. But what size hiatal hernia needs surgery? In this comprehensive guide, we will delve deep into the world of hiatal hernias to help you understand when surgery becomes necessary.
Understanding Hiatal Hernias
Before we explore the criteria for surgical intervention, it’s crucial to grasp the basics of what hiatal hernias are and the different types. Hiatal hernias primarily come in two forms:
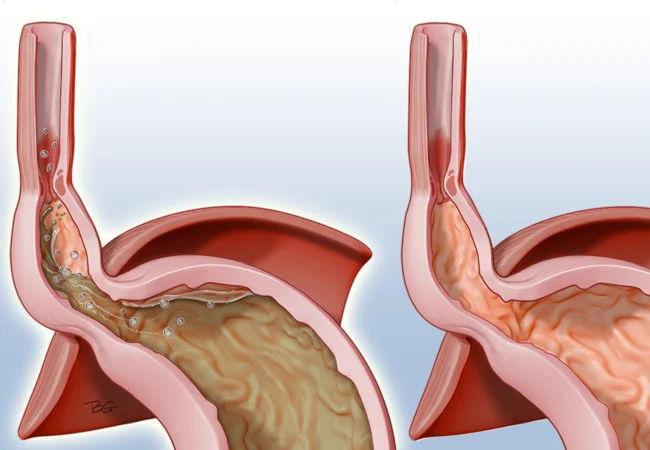
- Sliding Hiatal Hernia: This is the most common type of hiatal hernia, accounting for around 95% of cases. In a sliding hernia, a portion of the stomach and the gastroesophageal junction (where the esophagus meets the stomach) slide into the chest through the diaphragmatic hiatus, a small opening in the diaphragm.
- Paraesophageal Hiatal Hernia: This is a less common but potentially more serious type. In this case, the gastroesophageal junction remains in its normal position, but a portion of the stomach pushes through the diaphragm and sits next to the esophagus in the chest cavity. This type can lead to more severe complications.
The size of a hiatal hernia can vary considerably. Some are small and asymptomatic, while others can grow significantly and cause more pronounced symptoms. These symptoms can include:
- Heartburn
- Regurgitation
- Chest pain
- Difficulty swallowing
- Shortness of breath
- Vomiting blood
- Black, tarry stools (a sign of bleeding)
It’s essential to consult a healthcare professional if you experience any of these symptoms. Diagnosing the type and size of the hernia will be crucial in determining the most appropriate course of action.
Hiatal Hernia Sizes: When Does Surgery Become Necessary?
The size of a hiatal hernia is one of the key factors that doctors consider when deciding whether surgery is required. However, it’s not just the size alone that determines the need for surgical intervention. Other factors, such as the severity of symptoms and the patient’s overall health, play a crucial role in the decision-making process.
- Small Hiatal Hernias:
- Small hiatal hernias are often asymptomatic and don’t require surgery. Many people with small hiatal hernias may never even know they have one unless it’s discovered incidentally during tests for other conditions.
- These small hernias are typically managed with lifestyle modifications and medications to control symptoms, such as antacids and proton pump inhibitors (PPIs).
- Regular monitoring through medical check-ups may be recommended to ensure the hernia is not growing or causing new symptoms.
- Medium-sized Hiatal Hernias:
- Medium-sized hiatal hernias are generally more noticeable and may cause more pronounced symptoms.
- In some cases, surgery might be considered for medium-sized hernias, especially if lifestyle modifications and medications are ineffective in managing symptoms.
- The decision to perform surgery will depend on the patient’s overall health and the extent to which the hernia is impacting their quality of life.
- Large or Paraesophageal Hiatal Hernias:
- Large hiatal hernias and paraesophageal hernias are more likely to require surgical treatment due to the risk of complications.
- Surgery is often recommended to prevent severe complications like gastric strangulation, where blood flow to the herniated portion of the stomach is compromised, leading to tissue death.
- The risk of bleeding, severe reflux, and other complications is higher in these cases.
Choosing the Right Surgical Approach
When surgery is deemed necessary, the next step is to determine the most appropriate surgical approach. There are several options available, and the choice depends on the patient’s condition and the surgeon’s expertise. The main surgical procedures for hiatal hernia repair are:
- Laparoscopic Nissen Fundoplication:
- This is one of the most common surgical procedures for hiatal hernia repair.
- It involves wrapping the top of the stomach (the fundus) around the lower esophagus to prevent reflux and sliding of the hernia.
- Laparoscopic surgery is minimally invasive and typically involves smaller incisions and a shorter recovery period.
- Laparoscopic Toupet Fundoplication:
- Similar to the Nissen fundoplication, this procedure wraps the fundus around the lower esophagus but in a partial manner.
- It’s often recommended for patients with large hiatal hernias or those who have had previous failed anti-reflux surgeries.
- Laparoscopic Collis Gastroplasty:
- In cases where the esophagus is too short, a Collis gastroplasty may be performed to lengthen it.
- This procedure is often combined with a fundoplication to provide better support and prevent hernia recurrence.
- Open Surgery:
- In some cases, open surgery may be necessary, especially for complex, large, or recurrent hernias.
- Open surgery involves a larger incision and a longer recovery time, but it provides the surgeon with better visibility and access to the affected area.
Post-Surgery Recovery and Follow-Up
The recovery period after hiatal hernia surgery can vary depending on the type of surgery performed, the patient’s overall health, and other individual factors. In general, though, patients can expect the following:
- Hospital Stay: Most laparoscopic surgeries for hiatal hernias are performed on an outpatient basis or with a short hospital stay. Open surgery may require a longer hospital stay.
- Pain and Discomfort: Some post-operative pain and discomfort are normal. Pain management is typically provided to ensure patient comfort.
- Diet: After surgery, patients may need to follow a liquid or soft diet for a period before gradually transitioning back to regular foods.
- Activity: Patients are usually encouraged to resume light activities, such as walking, soon after surgery. However, strenuous physical activity may need to be avoided for a few weeks.
- Follow-Up Appointments: Regular follow-up appointments with the surgeon are crucial to monitor the healing process and assess the success of the surgery.
Conclusion
The decision to pursue surgery for a hiatal hernia is a complex one that depends on multiple factors, including the size of the hernia, the severity of symptoms, and the patient’s overall health. While small hiatal hernias can often be managed with lifestyle changes and medication, larger hernias and those causing severe symptoms may require surgical intervention.
If you suspect you have a hiatal hernia or have been diagnosed with one, it’s essential to work closely with a medical professional to determine the most appropriate treatment plan. Surgery, when deemed necessary, can provide relief from the discomfort and potential complications associated with hiatal hernias. Always consult with your healthcare provider to discuss your unique case and treatment options.