The term “tombstoning” is used to describe the phenomenon of losing a patient’s ECG during a cardiac arrest. The term was first coined by Dr. Paul Pepe at the University of Pennsylvania in 2006 and has since become a popular way to describe this phenomenon in the medical literature.
Dr. Pepe initially described tombstoning as a “spectral gap” in the ECG spectrum, which occurs when a patient experiences ventricular fibrillation (VF) or ventricular tachycardia (VT) during CPR. In these cases, chest compressions can be performed such that they occlude both ecg atrial and ventricular tissues; thus, no electrical signal can be detected from either chamber. This causes an interruption in the PQRST complex (more commonly known as QRS complex) that makes up the typical ECG trace.
Tombstoning is a phenomenon that occurs when a patient has been transferred from one bed to another, or when they are moved from the lateral decubitus position to the supine or upright position. This sudden change in posture causes the heart to momentarily stop beating, which can lead to ventricular tachycardia and ventricular fibrillation.
Tombstoning can also occur during general anesthesia, when the patient undergoes a sudden change in position from the supine to the prone position.
What is tombstoning in ECG?
What is tombstoning in ECG?
Tombstoning refers to the flat line appearance of the electrocardiogram (ECG) and is usually associated with a lethal arrhythmia. It can be caused by a number of conditions, including ecg cardiac arrest, asystole (no detectable heart rate) and ventricular fibrillation.
Tombstoning occurs when the electrical activity of the heart ceases for an extended period of time. This causes a loss of electrical signal from the electrodes on the skin surface that are ecg used to record an ECG trace. As a result, no visible deflections are seen on the ECG graph and it appears as if there has been a “cave-in” or “tombstone” ecg effect on the ECG trace.
Tombstoning is a feature of ECG where the ST segment is elevated and then falls to baseline in one or more leads. It can be seen in patients with pericarditis and some other cardiac conditions like Brugada syndrome.
What is the tombstone rhythm called?

The tombstone rhythm is a normal sinus rhythm with a short PR interval, a delta wave, and a tall R-wave in V1 through V3. This pattern can be seen in the presence of atrial fibrillation or atrial flutter.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia in patients older than 65 years and is associated with increased mortality and morbidity from stroke and heart failure. The prevalence of AF increases with age, affecting 5% to 8% of people aged 80 years and older.
The incidence of AF increases with age but remains relatively low in patients younger than 55 years. However, the risk for stroke is substantially higher in younger patients with AF compared with older patients. The incidence of AF is higher among men than women; however, this difference may be partly due to inherent differences between sexes or may be related to the different factors that predispose men and women to AF.
What is the ECG of MI?
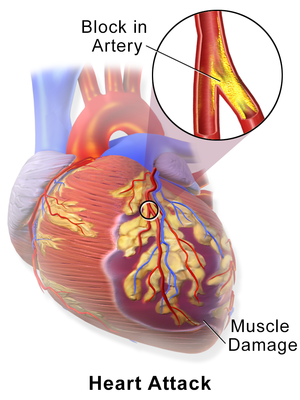
The ECG of MI is a characteristic pattern consisting of ST elevation and depression, representing myocardial ischemia. The ST segment is the level of the underlying myocardium. In MI, there is significant necrosis of the muscle fibers in a transmural pattern. The result is that the myocardium fails to contract properly and there is no blood flow through the region. This area will appear as an ST elevation or depression on the ECG.
There are three types of MI:
STEMI – Acute occlusion of a major coronary artery with complete occlusion of the vessel resulting in total blockage of blood flow to a portion of myocardium that requires urgent reperfusion
NSTEMI – Acute occlusion of a major coronary artery without complete occlusion such as plaque rupture with thrombus formation or spasm causing partial obstruction (nearly complete)
ST Elevation Myocardial Infarction (STEMI)
What are the 4 types of myocardial infarction?
The four types of myocardial infarction are:
ST segment elevation myocardial infarction (STEMI). This type of MI can occur in people without known heart disease. In this condition, the heart muscle is damaged and there is often a large amount of bleeding into the pericardium (the sac around the heart). The blood supply to the heart muscle is blocked by a clot that forms on an area of damaged tissue in one of ecg the coronary arteries. This area usually has a very high concentration of calcium deposits called ecg atheroma, which can rupture and cause clotting. If the clot becomes large enough to block all or part of an artery, it prevents oxygen-rich blood from reaching part or all of the heart muscle.
Nonsustained ventricular tachycardia (NSVT). This type of MI occurs when there is abnormal electrical activity in your heart’s ventricles (lower chambers) that causes your heartbeat to speed up for brief periods of time, but does not stop for long enough for your heart to beat normally again. It can last from several seconds to a few minutes, but it does not cause any permanent damage or symptoms.
Unstable angina pectoris (UAP). UAP can
Myocardial infarction (MI) is a medical condition in which some of the heart muscle dies due to a lack of blood supply. The damaged tissue becomes scar tissue and has lost its ability to contract. This can lead to heart failure, heart attacks and death.
There are four main types of MI:
• ST elevation MI (STEMI) – this type is the most common form of heart attack and occurs when the supply of oxygenated blood to the heart muscle is interrupted due to blockage of one or more coronary arteries by a blood clot.
• Non-ST elevation MI (NSTEMI) – this form of heart attack is less common than STEMI but still requires urgent treatment because it can lead to serious complications if left untreated. If a person has signs and symptoms of an NSTEMI, they will likely be treated with medication such as aspirin or clopidogrel, and then monitored regularly for signs of worsening heart attack symptoms such as chest pain or shortness of breath. If these symptoms worsen, they may need further treatment with drugs called thrombolytics or surgery.
• Unstable angina – unstable angina occurs when there is significant narrowing in one or more coronary arteries, but
What are 3 symptoms of a myocardial infarction?
A myocardial infarction, also known as a heart attack, is the death of heart muscle tissue due to a lack of blood flow. The most common symptom is chest pain or pressure, which can be mild or severe. Other symptoms may include shortness of breath, nausea or vomiting, and sweating.
The main triggers for a myocardial infarction are coronary artery disease and atherosclerosis. Coronary artery disease occurs when plaque builds up in the arteries that supply blood to the heart. Atherosclerosis is a buildup of fatty substances in these arteries that narrows them and reduces blood flow through them.
If you experience any of these common ecg symptoms and have risk factors for coronary artery disease, you should seek medical attention immediately:
Chest pain or pressure that lasts more ecg than two minutes
Pain spreading to your jaw, back or arms
Shortness of breath
Nausea or vomiting
Sweating
Which type of MI is most serious?
Myocardial infarction (MI) is a medical condition in which the blood supply to part of the heart muscle is interrupted. The interruption can be due to blockage or rupture of a coronary artery. This blockage is usually caused by occlusion of the coronary artery by a blood clot or plaque. Myocardial infarction (commonly shortened to MI) is often called a heart attack.
The severity of an MI depends on ecg which part of the heart muscle is affected, how much damage occurs, and how quickly treatment is received.
Myocardial Ischemia
The most common type of acute coronary syndrome (ACS) is myocardial ischemia, which occurs when your heart doesn’t receive enough oxygen-rich blood. Ischemia can occur ecg when your arteries narrow due to plaque buildup, or because you’re having chest pain and shortness of breath (angina). If you don’t get treatment right away, some areas of your heart may start dying off from lack of oxygen and nutrients — this process is called necrosis.
What is the most common type of myocardial infarction?
The most common type of myocardial infarction is the ST-elevation myocardial infarction (STEMI).
The second most common type is the non-ST-elevation myocardial infarction (NSTEMI).
A STEMI occurs when there is complete or partial blockage of one or more of the major arteries that supply blood to the heart. The decreased blood flow can cause chest pain, shortness of breath and other symptoms.
A NSTEMI occurs when there is some ecg damage to heart muscle, but not a complete blockage that would cause a STEMI. The amount of damage may vary from minor to severe depending on how many arteries are affected.
The most common type of myocardial infarction is caused by a blockage of one of the coronary arteries. The term “coronary” refers to the heart’s main arteries, which supply oxygen-rich blood to the heart muscle.
In this type of heart attack, which accounts for about 85% of cases, an artery that supplies blood to part or all of the heart muscle suddenly becomes blocked. This often happens when a clot forms in an artery and prevents blood from reaching part or all of the heart muscle.
In some cases, the clot breaks off from its own ecg plaque (a build-up of fatty material) and travels through the bloodstream until it lodges in an artery supplying blood to part or all of the heart muscle. In other cases, a large plaque develops over time and ruptures, releasing a clot that blocks an artery supplying blood to part or all of the heart muscle.
The remaining 15% of cases involve problems with your heart’s electrical system (circulatory shock), which can also cause sudden death if not treated immediately
What is the difference between Type 1 and Type 2 myocardial infarction?
The two main types of myocardial infarction are type 1 and type 2. A myocardial infarction occurs when blood flow to the heart muscle is blocked. The blockage can be caused by a buildup of plaque in the coronary artery or by a clot that forms in the coronary artery.
Type 1 or ST elevation MI: Occurs when there ecg are changes in the configuration of the heart muscle due to reduced blood supply. The electrical system of the heart, which generates an electrical impulse, goes into disarray. This causes a heart attack that requires immediate medical attention and treatment.
Type 2 or Non-ST elevation MI: Occurs when there is no apparent change in configuration of the heart muscle due to reduced blood supply. Only one part of the heart muscle is affected.
The type of heart attack you have depends on the location of the blockage.
There are two types of heart attack: ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI).
Type 1 (STEMI) heart attacks involve a complete blockage of one or more blood vessels in the heart. This is called a thrombosis, or clot. A STEMI usually requires emergency treatment with clot busting drugs and sometimes surgery to remove the clot.
Type 2 (NSTEMI) heart attacks involve a partial blockage of one or more blood vessels in the heart. They don’t usually require emergency treatment but may need more than one type of medicine for a long time.
There are two main types of myocardial infarction: ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI). The difference between the two is that STEMI is caused by a blockage of blood flow in one or more of the heart’s coronary arteries, while NSTEMI is caused by a lack of blood flow in one or more coronary arteries.
The blockages that cause these two ecg types of MI can be either stable or unstable. A stable lesion does not change over time and does not require immediate treatment, while an unstable lesion will worsen over time if left untreated.
Myocardial infarction (MI) is a disease of the heart muscle in which there is an insufficient supply of oxygenated blood. This can be due to coronary artery disease or other causes. In the United States, MI was the first leading cause of death for both men and women in 2008.[1] Acute myocardial infarction is a medical emergency that requires immediate treatment.
The two main types of MI are ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI).[2]
Both types of MI are treated with thrombolytic ecg therapy or percutaneous coronary intervention (PCI). The choice of treatment depends on whether a person has symptoms at the time of presentation.[3][4]
What is a Type 2 myocardial infarction?

A type 2 myocardial infarction (MI) is a heart attack caused by blocked blood flow to the heart. This blockage occurs when plaque builds up in an artery that supplies blood to your heart muscle.
A type 2 MI can be very serious and life-threatening, but it’s less common than a type 1 MI, which is the most common type of MI.
Signs and symptoms of a type 2 MI include:
Chest pain or pressure. The pain will usually start suddenly and may feel different from a typical chest pain. It’s usually located under the breastbone. Sometimes, people don’t have ecg chest pain with this type of MI. Instead, they might feel discomfort in their arms, neck, jaw or back instead.
Shortness of breath
Lightheadedness or dizziness
Sweating
A type 2 myocardial infarction (heart attack) is a heart attack caused by a clot that forms in the coronary artery. It’s also called a coronary thrombosis.
A type 2 myocardial infarction can happen when the walls of the arteries that supply blood to your heart muscle are damaged or blocked by a blood clot. When this happens, parts of your heart muscle may die because they don’t get enough blood.
The most common cause of death from a heart attack ecg is sudden cardiac arrhythmia resulting from an uncontrolled rise in blood pressure during physical exertion or anxiety (so-called widow-maker syndrome). Other causes include:
Coronary atherosclerosis – which results from cholesterol build-up on the walls of the coronary arteries, causing them to narrow and harden
Family history of premature heart attacks
High blood pressure – high blood pressure puts ecg stress on your arteries, making it easier for them to develop plaques and clots
High cholesterol levels – high levels of low-density lipoprotein (LDL) cholesterol increase your risk of developing atherosclerosis and having a heart attack
A type 2 myocardial infarction (commonly known as a heart attack) is the result of reduced blood flow to the heart muscle, caused by a blockage in one or more of its coronary arteries.
Blockages can be caused by atherosclerosis, the accumulation of fatty deposits on the inner lining of the artery walls. This process can be accelerated by smoking and poor diet, leading to narrowing of the arteries. If blood flow becomes severely reduced, it can cause injury to heart tissue and lead to angina (chest pain). If blood flow remains restricted for longer periods of time, permanent muscle damage may occur.
A type 2 myocardial infarction can also be caused by spasm or rupture of an atheroma that has not yet reached its full size (a “ruptured plaque”).
A myocardial infarction (MI) is a heart attack that occurs when the blood supply to part of the heart muscle is interrupted. It can be caused by coronary artery disease, which is the narrowing of the coronary arteries due to atherosclerosis. A MI can also be caused by other conditions such as cardiomyopathy (a disease that affects the heart muscle), or extremely rarely by damage to the heart’s electrical system.
There are two main types of MI: ST-elevation MI (STEMI) and non-ST-elevation MI (NSTEMI).
What is an ST-elevation MI?
An ST-elevation myocardial infarction (STEMI) is when there is an initial blockage in one or more of your coronary arteries that causes your heart muscle tissue to die. The damaged area needs oxygen, so your body sends more blood to it through vasodilation. This causes pain in your chest, which happens suddenly and continues for longer than 30 minutes, even after rest and aspirin treatment
What are the 3 most common complications of an MI?
What are the 3 most common complications of an MI
Heart attack (MI) is a heart condition that occurs when the blood supply to part of your heart is suddenly blocked. This can happen for many reasons, but the most common is coronary artery disease (CAD).
The heart muscle doesn’t get enough oxygen or nutrients and starts to die. If the damage is extensive enough, it can cause permanent damage to your heart muscle and may even lead to death.
Your heart will beat faster and harder to try and pump more blood around your body. But with less blood getting through your arteries, this puts a strain on your heart and can lead to complications.
There are three main complications that can occur after an MI:
Heart failure — when your heart isn’t able to pump enough blood around your body
Stroke — when there’s a sudden loss of blood flow in the brain due to a tear in an artery
Kidney failure — when one or both kidneys fail
What are the 3 most common complications of an MI?
- Heart failure
- Stroke
- Pericarditis